Medically reviewed by Dr. Seema Masrani, M.B.B.S.
Executive Summary
Autoimmune conditions are some of the most difficult conditions to handle: no common enemy, no single location and no unique mechanism of action. The supplements suggested:
Necessary:
Omega-3 oils: 1,000 mg a day;
Vitamin D: 2000 IU a day;
Curcumin: 500 mg a day;
Coenzyme Q10: 300 mg a day; and
Probiotics: 20 billion CFUs (colony-forming units) a day.
Optional:
B-vitamins;
Prebiotics or Fibre;
Glutathione;
Selenium; and
Zinc.
Disclaimer: The information, including but not limited to, text, graphics, images, and other material, contained on this website is for informational and educational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Autoimmune disorders develop when your body’s immune system mistakenly attacks and damages its own healthy tissues. The diseases are difficult to manage because science has a limited understanding of what causes them and how they progress. However, with good medical treatment, dietary and lifestyle changes and supplementation, they can be kept in check.
Unlike heart disease or diabetes, the layperson knows little about autoimmune disorders. The patients follow incorrect lifestyles and diets out of ignorance, aggravating the problem. In this article, I will discuss how a malfunctioning immune system causes these conditions and supplements that may help.
Introduction
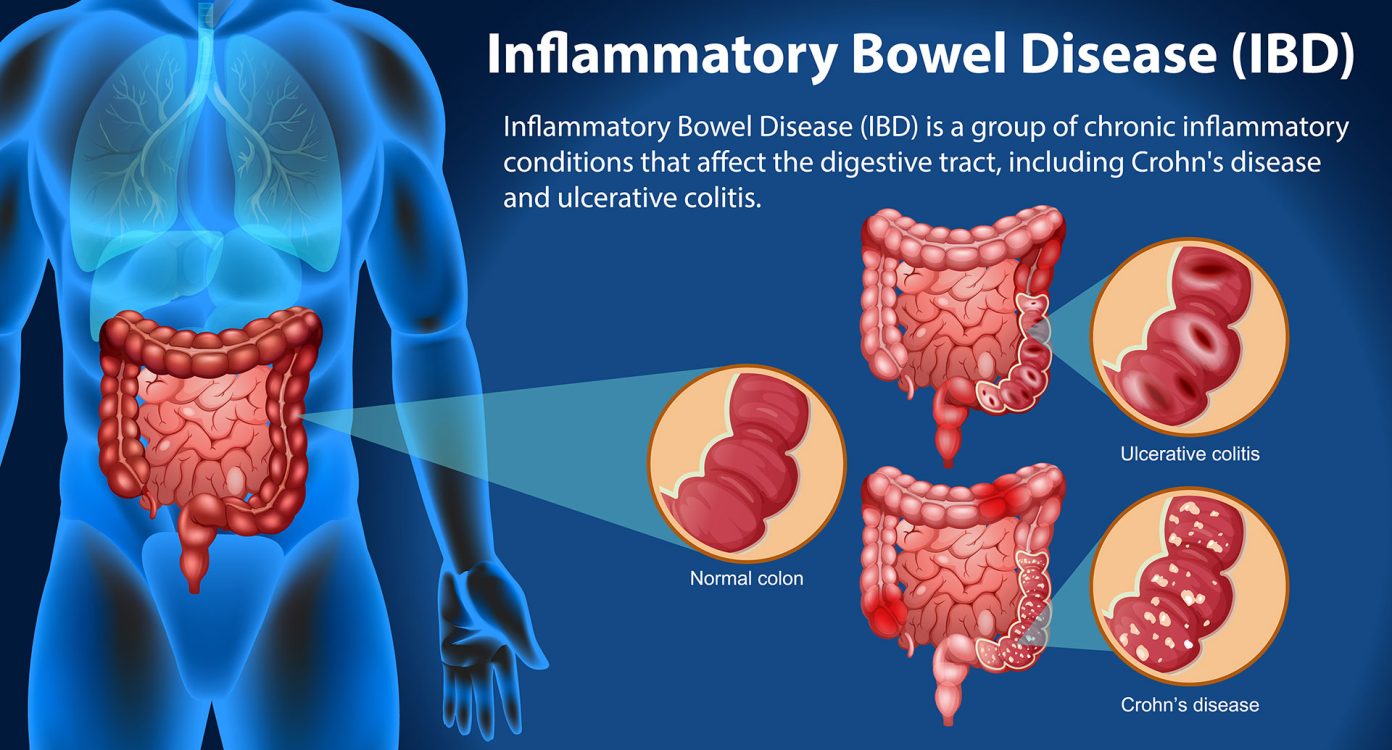
Autoimmune conditions include more than a hundred diverse medical disorders such as type 1 diabetes, hypothyroidism, psoriasis, rheumatoid arthritis and inflammatory bowel disease.
The name suggests why they are so hard to treat or control. Auto means self and immune refers to the body’s immune response. Autoimmunity is caused when your body’s immune system mistakenly attacks its own tissues. There lies the dilemma: If you suppress the immune system, the autoimmunity symptoms may subside but you will be more vulnerable to external enemies like microbes.
Below is an explanation of our immune system’s functioning. It is intricate, a reason why very few people understand it properly. You don’t need to know it to address your autoimmune condition; however, it will clear some misconceptions and lay out your options. If you don’t care about the details, skip to the Medical Management of Autoimmune Conditions subsection.
Our Immune System
During the Covid pandemic, you learned how your immune system defends against external attackers such as the SARS-CoV-2 virus. It performs three main tasks:
- Identify the body’s enemies
- Destroy them and
- Remember them.
Let us discuss them one by one.
Identifying the Body’s Enemies
Your immune cells travel around the body searching for entities harmful to their owner: you. As the cells can’t see anything, they distinguish each object by identifying its chemicals.
The immune cells sniff for distinct proteins in the cells they encounter. But they can’t perform chemical analysis like we do in our labs. Instead, the cells use the Cinderella’s Shoe logic: In the folk tale, the prince goes around searching for Cinderella but since he cannot tell what Cinderella looks like (hey, it is a fairy tale), his only tool is the glass shoe she had left behind. He asks every young woman to wear the shoe and the lady whose foot fits inside the shoe is deemed Cinderella!
Similarly, the immune cells carry specialised proteins on their surfaces that act like a unique shoe. They try to attach the parts of those proteins to the proteins on the items they encounter. If the two contours fit, the cells know the identity of the other protein and its carrier cell. The protein appendages on the immune cells are called receptors and like gloves, they fit only specific protein shapes, helping identify them.
But how can that be foolproof — someone else may have the same foot size and shape as Cinderella’s? Indeed, the immune system goes wrong occasionally. For example, your heart cells have proteins similar to those in bacteria that cause strep throat or scarlet fever. After such an infection, your immune system tries to search and destroy all bacteria that caused it but in the process, mistakenly thinks that your heart cells are also those bacteria and attacks them, causing rheumatic heart disease.
So what are the enemies of your body? Now it starts getting complicated.
The Enemies of Your Body
Not all bacteria and viruses are bad; some are required for good health. Some of the body’s own cells can be cancerous and dangerous. Here is the list of bad guys:
- Most bacteria and viruses
- Many toxic chemicals and
- Body cells that have turned cancerous.
At the same time, the immune system has to ensure that the following good guys are not attacked:
- Your body’s all normal cells
- Some bacteria in your intestines, mouth, scalp and other body parts, where they live in a symbiotic relation with your body (they feed on the nutrients in your body and in turn, they perform tasks valuable to your body such as making B-vitamins or preventing harmful pathogens from colonising your body) and
- The foetus, which has cells genetically different from its mother’s.
Antigens
The identifying chemicals that the immune cells check for are called antigens. They may be inside a cell, on its surface (bacteria or cancer cells) or as a part of its genetic material (viruses).
Our body cells have different antigens than those on external microorganisms. Cells of some of our organs, such as heart cells, have additional antigens. This helps immune cells to distinguish cells in more detail.
Most medical literature defines antigens as substances that can trigger an immune system reaction in the body. But that is not correct. For example, small molecules called hapten are antigens that do not invoke an immune response. The antigens that activate an immune reaction are called immunogens.
Destroying the Body Enemies
The immune cells know which antigens are safe and which belong to harmful entities. To eliminate the enemy cells or toxins, the immune system uses various mechanisms, the main one being Antibody Production.
Antibodies
When an immune cell detects a harmful antigen, it quickly replicates itself into numerous clones. Those cells manufacture and release billions of identical protein molecules called antibodies specific to that antigen into the bloodstream.
Antibodies neutralise the antigens by attaching to them. An antibody that binds to an antigen on a toxin’s surface is called an antitoxin and causes enough chemical changes in the toxin to make it inactive. Some antibodies make a bacteria immobile by attaching to its antigen. Some others bind to a bacteria attracting certain scavenger cells who eat that bacteria. A few antibodies coat the antigens on bacteria such that certain blood chemicals rupture the bacteria’s membrane killing it.
The immune cells make enough antibodies that every single antigen molecule in the body is destroyed over a few days. Additional antibodies can float in the blood fluids for years, offering the body immunity against that antigen and its owner: the enemy.
Remembering the Body’s Enemies
When a previously unknown enemy pathogen enters the body, the immune system needs many days until it can launch a full-fledged immune attack against that enemy. This happened when the SARS-CoV-2 virus afflicted us for the first time. But since there is a risk that an invading microbe can overwhelm the body’s defences quickly, the immune system needs a way to gear up quickly for the attack. So it has a learning mechanism to do so if the same enemy invades again.
After destroying the enemy, some immune cells retain parts of its antigen proteins. They circulate in the blood for months or years, acting as a reference for our immune system about that parasite’s antigen. If the same microbe attacks the body again, our immune system can match the antigens on that microbe’s surface with this reference and gear up quickly to stop that enemy.
Collecting the Enemy Records
Every new pathogen attack ends with a few immune cells carrying its antigen’s record. Over time, the immune system gathers a collection of such ‘reference’ cells – it has learned about the enemies it has fought and how to deal with them in the future.
Vaccination
Vaccination helps create such new records without a risk of severe infection. Some references float in the blood for your entire life and others fade away after some duration, an outcome that depends on the antigen. That is why you need a flu vaccine every year, a typhoid vaccine every two years, a tetanus vaccine every ten years and a measles vaccine only once in your life.
Weak Immune System
Your immunity reduces when you are stressed, sleep-deprived, nutrient-deficient or suffering from some illness. If your immune system is underactive or weak, it won’t be able to kill pathogens, destroy toxins or eliminate cancer cells correctly, making you vulnerable to infections and various cancers.
In a healthy body, nearly one million cells turn cancerous every day. In trillions of our body cells, energy is produced continuously. Such reactions are inherently degenerative (oxidative and inflammatory) and can alter the cell’s DNA causing genetic mutations. Most changes are so extreme that the cell severely malfunctions and dies. But in about a million cells daily, the damage is not enough to kill the cell but sufficient to make it behave erratically. Read on this website: Your genetic blueprint: Genome, chromosomes, DNA, and genes.
A healthy immune system figures out which cells are misbehaving and kills them. But when immunity is low, a few of them escape destruction and grow into cancer tumours. That is why prolonged periods of poor immunity are potentially dangerous.
Other reasons may also cause low immunity. There could be some genetic factors. Steroid medicines reduce your immune cells’ activity. Some bone marrow or organ transplant patients are given immunosuppressant medicines to improve the acceptance chances of the outside tissues. Finally, pathogens such as the human immunodeficiency virus or HIV may cause low immunity. Except when lowered by doctors as a part of some treatment, low immunity is not good.
Overactive Immune System
While low immunity is bad, overactive immunity is not necessarily good. High immunity is desirable only if the immune system is functioning properly. A faster car is preferred if the roads are in good condition. Otherwise, higher speeds may cause an accident.
If a hyperactive immune system malfunctions, it can cause two problems: hypersensitivity and autoimmunity. To understand them, we need to learn the concepts of self-antigen and immune tolerance.
Self-Antigens
Antigens on your body’s own cells are called self-antigens. A healthy immune system should be able to tell apart self-antigens and not attack them.
You can think of antigens as the ID cards in an office. Company personnel have their ID cards while the visitors have separate credentials, authorising them on the premises. The security staff goes around, verifying everyone’s ID papers and those who don’t have the approved ones are considered intruders and appropriately dealt with.
This is roughly what your immune system does; but in a roundabout way through immune tolerance.
Immune Tolerance
Your immune cells don’t quite sniff and ignore self-antigens. Different immune cells destroy distinct antigens but your immune system either kills or makes unresponsive the immune cells that could attack self-antigens or antigens of desirable gut bacteria. This toning down of immune response to specific antigens is called immune tolerance.
To rewrite the previous analogy, there are different security guards for each type of ID issued: employee cards, visitor cards, etc. All of them beat up (or whatever is politically correct) their respective candidates if they come across. However, the security staff that could verify and attack the company employees are either ‘killed’ or made inactive so that the company’s employees don’t get harmed.
This is called negative selection — instead of making only the cells that destroy the enemies, the body manufactures all kinds of cells that respond to each entity and then out of them, destroys those that attack your body cells. Sounds convoluted? Well, that is how life works.
Read:
• Immune Tolerance Network: Immune Tolerance in Autoimmune Disease
• Akadeum Life Sciences: What is Immune Tolerance and Types of Immunological Tolerance
Evolution and Immune Tolerance
As a philosophical aside, how did nature come up with such a complex mechanism? Living beings have come this far along the development tree because nature performs trials and errors. They produce outcomes that are almost always worse but rarely, superior to the existing life. Such ‘mutants’ thrive better than their original counterparts. In the long term, over billions of iterations, the hardier lifeforms sustain: the survival of the fittest. That is the evolution for you. Immune tolerance is the way the body decides to ignore the self and destroy its enemies.
Ageing and Immune Tolerance
With age, the immune system accumulates a catalogue of different enemy antigens and gets better at repelling more types of enemies. In the process, though, some immune cells inadvertently collect the body’s own antigens (called self-antigens or auto-antigens) on their surfaces. Such an immune system thinks that your own antigens are enemy antigens. It is like police records erroneously listing your photo as a criminal. Without immune tolerance, the chances of your immune system wrongly attacking your own body tissues will increase with age.
Why is this complicated discussion important? Just for a single point: Autoimmune conditions don’t develop because an immune system becomes too strong; they do because it loses its immune tolerance.
Loss of Immune Tolerance
Under certain conditions, your body can lose immune tolerance. The consequences are immense:
- If your body loses tolerance to self-antigens, it can develop an autoimmune disorder.
- If your body loses tolerance to food or pollen antigens, you will develop hypersensitivity or allergies.
- If your body is fooled by certain pathogens into developing tolerance towards their antigens, your body cannot kill them ever (immune escape)
- If your body is fooled by certain tumour cells to develop tolerance towards their antigens, they can grow unchecked and become full-fledged cancers (tumour escape)
Low Immunity versus Immune Tolerance
Immune tolerance is different from weak immunity or immunity suppression. Immune tolerance is specific to an antigen, while low immunity applies to all antigens. Immune tolerance is normal and by design; low immunity is an abnormal condition.
Low immunity may cause infections as pathogens may not get killed. On the other hand, normal immunity with an incorrectly developed immune tolerance for certain bacteria may lead to that specific infection as your body cannot get rid of it.
Low immunity may allow many types of cancers to flourish. On the other hand, normal immunity with undesired tolerance to certain tumour cells will allow that specific cancer to develop.
Finally, immunity suppression involves induced tolerance, where the immune system is manipulated to avoid rejecting the transplanted organ. This is also a way to guard against severe allergic reactions.
High Immunity versus Autoimmunity and Hypersensitivity
High immunity does not make your immune cells go into overdrive destroying the wrong set of cells such as the body’s tissues. The additional condition needed is the loss of immune tolerance to that specific antigen.
If the immunity is high (or normal) but the system loses immune tolerance to self-antigens, the immune cells attack the body’s tissues causing autoimmune conditions.
If the immunity is high (or normal) and the system loses immune tolerance to certain antigens of allergens like pollen or toxins, your system shows hypersensitivity to that allergen and you develop allergy — hypersensitivity is an immune response, while allergy refers to a set of symptoms. For the technically minded, there are nonallergic hypersensitivity reactions, too, but that hardly matters for this article.
Read:
• HealthDirect: Allergies and hypersensitivities
• Medical News Today: What to know about the different types of hypersensitivity reactions
The important point to keep in mind is:
Supplements that boost immunity cannot cause autoimmunity or hypersensitivity because they do not affect immune tolerance.
Let us understand how our body can lose immune tolerance and develop autoimmune conditions.
How Various Autoimmune Conditions Develop
Science still does not know why and how our immune system loses some of its tolerance to self-antigens. But we can discuss some possibilities based on a few associations and circumstantial evidence.
Genetics
Genes can predispose one to develop autoimmune conditions, which does not mean one will contract those diseases. It needs environmental triggers to initiate the process. In a way, genes lay down a fertile ground but you need a seed to get a tree growing. The latter part is often an environmental trigger.
- Autoimmune diseases run in families.
- Genetically identical twins have a 25 to 50 per cent chance of getting the same autoimmune disease. Genetically non-identical fraternal twins have a two to eight per cent chance of getting the same autoimmune disease.
- There is no single gene that causes all autoimmune disorders. Distinct genes are involved in different conditions. Plus, autoimmune conditions are considered to be multifactorial—caused by a combined effect of multiple factors.
Read on the Johns Hopkins Medicine website: How do autoimmune diseases unfold?
Hormones
Women have a much higher chance of developing autoimmune conditions. For example, rheumatoid arthritis affects thrice as many women as men. But then, they also have a stronger immune response to vaccines and infections than men do. One guess is the role of female sex hormones such as oestrogens in immune function.
Infections
Strep throat is a bacterial infection that can give you a sore throat. An antigen on those bacteria resembles one on human heart cells. After the body clears strep throat infection, it retains that record. Later, it may mistakenly think that our body’s heart cells are a new strep throat infection and attack them. This can lead to rheumatic heart disease, an autoimmune condition.
Stress
Stress is caused by threat perception. This leads to a fight-or-flight response—a survival act. As the body gears up for those two possibilities, it tones down various body systems that are not essential for them, the immune system being one of them.
A stressed body releases stress hormones such as cortisol and norepinephrine, which suppress the immune system. In acute or extreme stress, we get an immune system disruption, triggering autoimmune conditions. We know that individuals with stress-related disorders are:
- More likely to be diagnosed with an autoimmune disease;
- More likely to develop multiple autoimmune diseases; and
- If they are undergoing treatment for stress-related disorders, the rate of developing autoimmune diseases is less than if they are not taking treatment.
Read:
• WebMD: Severe Stress May Send Immune System Into Overdrive
• Harvard Medical School: Autoimmune disease and stress: Is there a link?
Nutrient Deficiencies
Deficiencies of nutrients such as vitamin A, B vitamins, vitamin D, vitamin K2, omega-3 oils, magnesium, iron, selenium, and zinc are associated with autoimmune conditions. We don’t know if the deficiencies directly cause them but autoimmune conditions being multifactorial, a nutrient deficiency may trigger or worsen an autoimmune condition or prevent it from going into remission.
Damage Theory
If a normal body cell is altered by medicine, a virus or even sunlight, the immune system may confuse it as a foreign substance. The virus-infected cells may cause the immune system to attack that body part. If a tendon or a joint is constantly stressed and comes in contact with blood, an immune response may be triggered causing an autoimmune condition.
Food Allergies
New evidence suggests that there is a connection between autoimmunity and hypersensitivity. That is, if someone develops allergies, the individual also is likely to develop autoimmune conditions.
Many food additives in processed foods such as fat solvents and organic acids can lead to autoimmune conditions. This suggests a possible pathway through a damaged digestive system leading to a disorder called leaky gut syndrome.
Leaky Gut Syndrome
Eighty per cent of our immune system is in the lining of our digestive system. The healthy bacteria in the intestines are in a symbiotic relationship with our body. They produce many healthy chemicals that help in mood, metabolism and immunity. Covering their functions is a vast topic in itself. Read on this website: Microbiome: The other ‘You’.
Our intestinal lining is made of cells packed tightly together with tiny gaps in between them. They allow only certain substances, such as digested food nutrients, to reach the bloodstream from the gut.
Due to various reasons, this gut lining can get damaged causing leaky gut syndrome. The small intercellular gaps become larger, allowing big and harmful substances to enter the blood circulation. Some of these substances are undigested food particles, bad bacteria, toxins and large molecules such as gluten.
Once those substances enter the bloodstream, the immune system thinks of them as new invaders. It starts generating inflammation to neutralise them. However, the leaky gut keeps ‘leaking’ such substances into the blood with every meal.
Over time, the immune system catalogues such substances as ‘old’ invaders as it gets their antigen records. So the immune system attacks become stronger. But since the supply of these invaders is continuous from the leaky gut, the battle goes on. At some point, the immune system starts malfunctioning and causes autoimmunity.
The exact mechanism is still unknown, but many factors that trigger leaky gut syndrome are also implicated in autoimmune conditions, suggesting that the former causes the latter. For example:
- Vitamin D deficiency
- Acute stress
- Bacterial, fungal and viral infections
- Processed foods: Gluten, dairy, sugars, grains
- Exposure to toxins (chemicals, pesticides, air pollution, chemotherapy)
- Antibiotics, acidity or heartburn medicines (PPIs and acid blockers), painkillers (NSAIDs).
Locations of Autoimmune Diseases
In autoimmunity, the immune system releases destructive chemicals — antibodies — against self-antigens or auto-antigens in the bloodstream. So they are called auto-antibodies. Since an antibody is specific to an antigen, different auto-antibodies cause different autoimmune conditions.
Some autoimmune conditions affect the whole body, while others are localised to an organ:
- Rheumatoid arthritis: the antibodies attach to the linings of the joints;
- Inflammatory bowel disease: the antibodies attach to the linings of the intestines;
- Systematic lupus erythematosus or SLE: the antibodies attach throughout the body;
- Myasthenia gravis: the antibodies attach to neuromuscular junctions;
- Multiple sclerosis: the antibodies attach to the linings of the nerve cells of the brain and spinal cord; and
- Type 1 diabetes: the antibodies attach to insulin-producing beta cells in the pancreas.
Once the antibodies are attached to a cell, the immune system launches its attack on that cell, organ or location causing destruction.
So in autoimmune conditions, there is no fixed enemy, no unique location and no single mechanism. There is too much variation in the cause and progression of different autoimmune conditions. We are left with very few options for their treatment.
Medical Management of Autoimmune Disorders
You must consult your doctor for autoimmune conditions. But I want to give you some idea about the options available in modern medicine for autoimmune conditions.
As per modern science (allopathy), there is no cure for autoimmune conditions. Read Cleveland Clinic: Autoimmune Diseases. The treatment choices are limited. So as I mention supplements below, you should not have unreasonable expectations from them. Also, please check with your doctor before using any supplements.
- Allopathy uses medicines that suppress the immune system (immunosuppressants) such as methotrexate, azathioprine and mycophenolate. Since the immunity is artificially lowered, the patient has an increased risk of other infections and cancers.
- One may also use corticosteroids such as prednisone that reduce inflammation and immunity. They should be used for short periods but in some cases, one needs to use them indefinitely. The choice is of a lesser evil.
- In some conditions, biologic agents such as infliximab and adalimumab are used. They reduce the actions of another inflammatory marker or chemical called TNF-alpha.
- Some other medicines reduce the actions of white blood cells, which are involved in immune reactions.
- Then, there is a procedure called plasma exchange where blood is withdrawn, filtered to remove some abnormal proteins and returned.
- Finally, a procedure called intravenous immune globulin is used where a purified extract of certain chemicals taken from the blood of a volunteer donor is injected into you. We don’t know why and how it works.
Supplementation Strategies for Autoimmune Disorders
The non-invasive medical options are to reduce immunity (risk-prone) and inflammation (not so risky). Therefore, it may be a good idea to control inflammation with supplements. Anything that lowers immunity should only be done under a doctor’s guidance, not using supplements.
My supplementation approach would be to:
- Reduce inflammation caused by autoimmune conditions.
- Help regularise the body’s immune system response to autoimmunity.
- Give antioxidant support to the cell’s defence systems.
- Support the nervous system to respond to autoimmune condition demands.
Finally, note that autoimmune conditions are tenacious problems needing years of careful handling. So be prepared to persist with a very long-term and perhaps lifetime of use of supplementation. Since you are ready to use medicines for life, you might as well consider taking supplements along with them.
Also, do not ignore dietary and lifestyle changes that go a long way in preventing the progression of the disease. I have provided many links at the end. Do read those articles.
Some supplements are useful for a specific autoimmune condition such as rheumatoid arthritis but not others. I have left out such details since there are too many to mention.
Supplements to Reduce Inflammation
Chronic and excessive inflammation is a common thread in all autoimmune conditions. High inflammation creates a vicious circle by further revving up the immune system, which creates more inflammation. Lowering inflammation also reduces organ degeneration.
Omega-3 oils: Anti-inflammatory. Reduces the risk of developing rheumatoid arthritis. Reduces the risk of inflammatory arthritis in some patients. 1000 mg of EPA+DHA a day. Read on this website: Omega–3 oils: A complete guide.
Curcumin: Four per cent extract of turmeric. Improves rheumatoid arthritis, multiple sclerosis, psoriasis, and inflammatory bowel disease. Reduces inflammatory cytokines (signalling chemicals released by immune cells that cause inflammation).
Supplements to Regulate Autoimmunity
Frankly, we don’t know how some nutrients can regulate autoimmunity, but we know they do.
Vitamin D: Patients having type 1 diabetes, lupus, inflammatory bowel disease, hypothyroidism, and multiple sclerosis have vitamin D deficiency. Vitamin D regulates many parts of autoimmune activities, such as specific gene expressions (certain genes becoming active) and inflammatory markers (toxic chemicals released in the body). Five years of use of vitamin D was found to reduce the risk of developing autoimmune conditions by 30 per cent. Take 2000 IU a day.
Selenium: Regulates immunity. Reduces thyroid auto-antibodies (helps autoimmune hypothyroidism). Several selenoproteins (proteins containing selenium) are antioxidants.
Zinc: Regulates the immune system. Zinc deficiency is found in many autoimmune conditions.
No one knows if selenium and zinc supplementation will improve autoimmune conditions as there are no such studies done. But they might be worth taking given the ancillary evidence.
The evidence about the benefits of iron and magnesium in autoimmune conditions is conflicting. They are helpful for normal immune function. Their low levels can reduce immunity. However, the use of magnesium and iron in autoimmune conditions is found to be detrimental. Avoid taking extra amounts.
Supplements to Reduce Oxidative Stress
Glutathione: A highly potent antioxidant that is the main component of the cell defence system against free radical damage to cell mitochondria. It stimulates or reduces the immune response to control inflammation, as needed.
Polyphenols: These are components of plants, such as green tea and grapes. They help relieve painful symptoms of various autoimmune diseases. Consider supplements of antioxidants such as EGCG (green tea) and resveratrol (grapes).
Coenzyme Q10 or CoQ10: Has a therapeutic role in autoimmune conditions, such as rheumatoid arthritis, multiple sclerosis, and type 1 diabetes. It protects cell mitochondria from oxidative damage. Read on this website: Coenzyme Q10: A complete guide.
Supplements to Support Nervous System
Your digestive system controls 80 per cent of your immune system. It is also considered your second brain and has a big role in your nervous system. Plus, leaky gut syndrome is one trigger for autoimmune conditions. So keeping your digestive nervous system (called the enteric nervous system) healthy will help with autoimmune conditions.
Probiotics: These are foods or supplements containing healthy strains of gut bacteria. They help in autoimmune conditions through many mechanisms. Read here: Probiotic Applications in Autoimmune Diseases.
Prebiotics: These are dietary fibres in water-soluble and water-insoluble forms. They are foods for gut bacteria. Adequate amounts of them help keep the gut microbiome healthy.
B-vitamins: They are nutrients for the gut microbiome. They also regulate immune cell activity in the intestines. Read on this website: Everything you want to know about B–vitamins.
Omega-3 oils: They help maintain a balance between intestinal immunity and the gut microbiome. They maintain the intestinal wall integrity, affecting immune cells.
Siberian Ginseng: Advised for individuals who have chronic stress. It is an adaptogen, a compound that helps reduce stress response. Controlling stress through mindfulness and yoga is a lifestyle modification. But if one cannot reduce stress by behaviour modification, taking adaptogens is an indirect way — reduce the stress response, if not stress.
Ashwagandha: An adaptogen, used for thousands of years in Ayurveda, the Indian medicinal science. For individuals who have chronic, high stress.
To Read More
- MSD Manual: Autoimmune Disorders
- WebMD: What Are Autoimmune Disorders?
- Antioxidants Journal: Nutraceuticals against Oxidative Stress in Autoimmune Disorders
- Johns Hopkins Medicine: Autoimmune Disease: Why Is My Immune System Attacking Itself?
- Children’s Hospital of Philadelphia: What Happens When the Immune System Does Not Work Properly?
- Regeneration Health Medical Center: 5 Supplements For Your Autoimmune Disease
- The CSR Journal: 10 Steps To Reverse Autoimmune Diseases
- WebMD: Life with an Autoimmune Disease
- Immunopaedia.org: Central & Peripheral Tolerance
- NewScientist: Autoimmune Diseases May Be Side Effect of a Strong Immune System
- Pharmacy Times: Omega-3 Fatty Acids Promote Gut Health
Articles in Nutrients Series
- Omega–3 Oils: A Complete Guide
- Vitamin D: A Complete Guide
- Vitamin A: A Complete Guide
- Coenzyme Q10: A Complete Guide
- Turmeric (Curcumin): A Complete Guide
- Lutein: A Complete Guide
Articles in Supplementation Series
- Why Do We Need Supplements?
- Supplements for Various Age Groups
- Supplements for Preventing Ageing & Age-Related Diseases
- Supplements for Type 2 Diabetes
- Supplements for Osteoarthritis
- Supplements for Hair Loss
- Supplements for Fatty Liver
- Supplements for Autoimmune Disorders
- Supplements for Anemia
- Supplements for Prostate Enlargement
- Supplements for Macular Degeneration
- Supplements for PCOS
- Supplements for Parkinson’s Disease
- Supplements for Gout
- Supplements for Eczema
First published on: 22nd May 2022
Image credit: Image by Freepik
Last updated on: 28th December 2024

